
Access treatment effortlessly without the need for in-person appointments
Effective psoriasis treatments to manage symptoms and minimize flare-ups
At Online Chemist, we provide a variety of effective psoriasis treatments to help alleviate symptoms and improve skin health. Our selection includes calming emollients and targeted corticosteroids designed to reduce itching, redness, and inflammation. With a seamless online ordering process, you can conveniently access the care you need from home. Buy psoriasis treatment online today for fast, dependable service and expert-approved solutions to restore your skin.








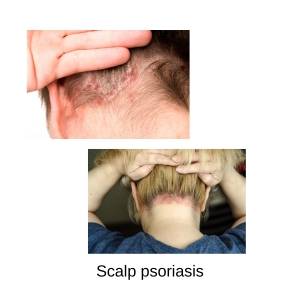
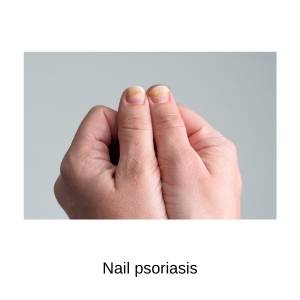
Psoriasis is a common, long-term skin condition that causes red, scaly patches, known as plaques, to form on the skin. These plaques are often itchy and can appear anywhere on the body, but they’re most commonly found on the scalp, elbows, knees, and lower back. In some cases, psoriasis can also affect the nails and joints.
Psoriasis affects both men and women and can start at any age, including childhood. However, it most commonly begins between the ages of 15–25 and 50–60. About one-third of people with psoriasis have a family history of the condition, suggesting a genetic link.
Psoriasis is considered an immune-mediated genetic skin disease. This means that the immune system mistakenly attacks healthy skin cells, leading to rapid skin cell production and the formation of plaques. Factors such as stress, skin injuries, certain medications, and infections can trigger or worsen psoriasis.
Here’s a simple overview of the types of psoriasis to help you understand:
Struggling with psoriasis?
Let us help you find relief with expert advice and personalised treatment
plans—all from the comfort of your home.
✅ Consult with Online Specialists
✅ Tailored Treatments for Your Needs
✅ Delivered Right to Your Door

Several factors can aggravate psoriasis or trigger flare-ups. These vary from person to person, but some common aggravating factors include:
Understanding and avoiding triggers can significantly improve psoriasis management and reduce flare-ups.
Take the first step toward clearer, healthier skin with our trusted online psoriasis treatment service.
✅ Consult with Online Specialists
✅ Tailored Treatments for Your Needs
✅ Delivered Right to Your Door
The treatment of psoriasis aims to control symptoms, reduce flare-ups, and improve the patient’s quality of life. While there is no cure for psoriasis, treatments are tailored based on the type, severity, and location of psoriasis, as well as individual patient factors.
Here’s an overview of treatment options:
Best for mild to moderate psoriasis or as adjunctive therapy for severe cases.
Effective for moderate to severe psoriasis, especially when topical treatments fail.
a. Narrowband UVB – The most common and effective phototherapy. Reduces inflammation and slows skin cell turnover.
b. PUVA (Psoralen + UVA) – Combines UVA light with psoralen (a photosensitizing agent). Used for more resistant cases but may increase the risk of skin aging and cancer.
c. Excimer Laser – Targets specific areas with high-dose UVB light. Useful for localized plaques on areas like the scalp or hands.
Used for moderate to severe psoriasis or when other treatments fail.
b. Biologic Therapies – Target specific parts of the immune system, such as cytokines like TNF-alpha, IL-17, and IL-23. Administered via injection or infusion. Highly effective for severe psoriasis and psoriatic arthritis.
c. Small Molecule Drugs – Apremilast: A PDE4 inhibitor taken orally to reduce inflammation. Fewer side effects compared to biologics.
Combines multiple treatment modalities (e.g., topical + phototherapy or systemic + biologics). Helps maximise effectiveness and minimise side effects.
Lifestyle Changes: Quitting smoking, reducing alcohol consumption, and maintaining a healthy weight can improve overall health and potentially reduce psoriasis severity.
Struggling with psoriasis?
Let us help you find relief with expert advice and personalised treatment
plans—all from the comfort of your home.
✅ Consult with Online Specialists
✅ Tailored Treatments for Your Needs
✅ Delivered Right to Your Door
Don’t simply rely on our claims, become part of the delighted community of thousands of customers who are experiencing the remarkable benefits!
Online Chemist
82 Middleton Road
Gorleston
Great Yarmouth
Norfolk, NR31 7AH
Phone: 01493 600610
Email: info@onlinechemistuk.net
Superintendent Pharmacist:
Obaidullah Zaman
BPharm, MPharm, PGDip (Pharmacy), MRPharmS, IP
GPhC Reg. Number: 2083409
Pharmacy Premises GPhC Reg. Number: 9011159
Monday 09:00 – 17:00
Tuesday 09:00 – 17:00
Wednesday 09:00 – 17:00
Thursday 09:00 – 17:00
Friday 09:00 – 17:00
Saturday Closed
Sunday Closed
Click here for driving directions
OnlineChemist is a trading name of Nomaz Limited.
Registered in England – 11349276.
© 2025 All rights reserved.